Frozen shoulder disease or adhesive capsulitis is a painful inflammatory condition in which the shoulder becomes stiff. Treatment options aim to control pain and restore strength to the shoulder joint.
What is frozen shoulder disease?
The shoulder joint, which is called the “ball and socket” joint, consists of three bones; The upper part of the humerus, which forms the ball, moves into the socket formed by the edge of the scapula and clavicle.
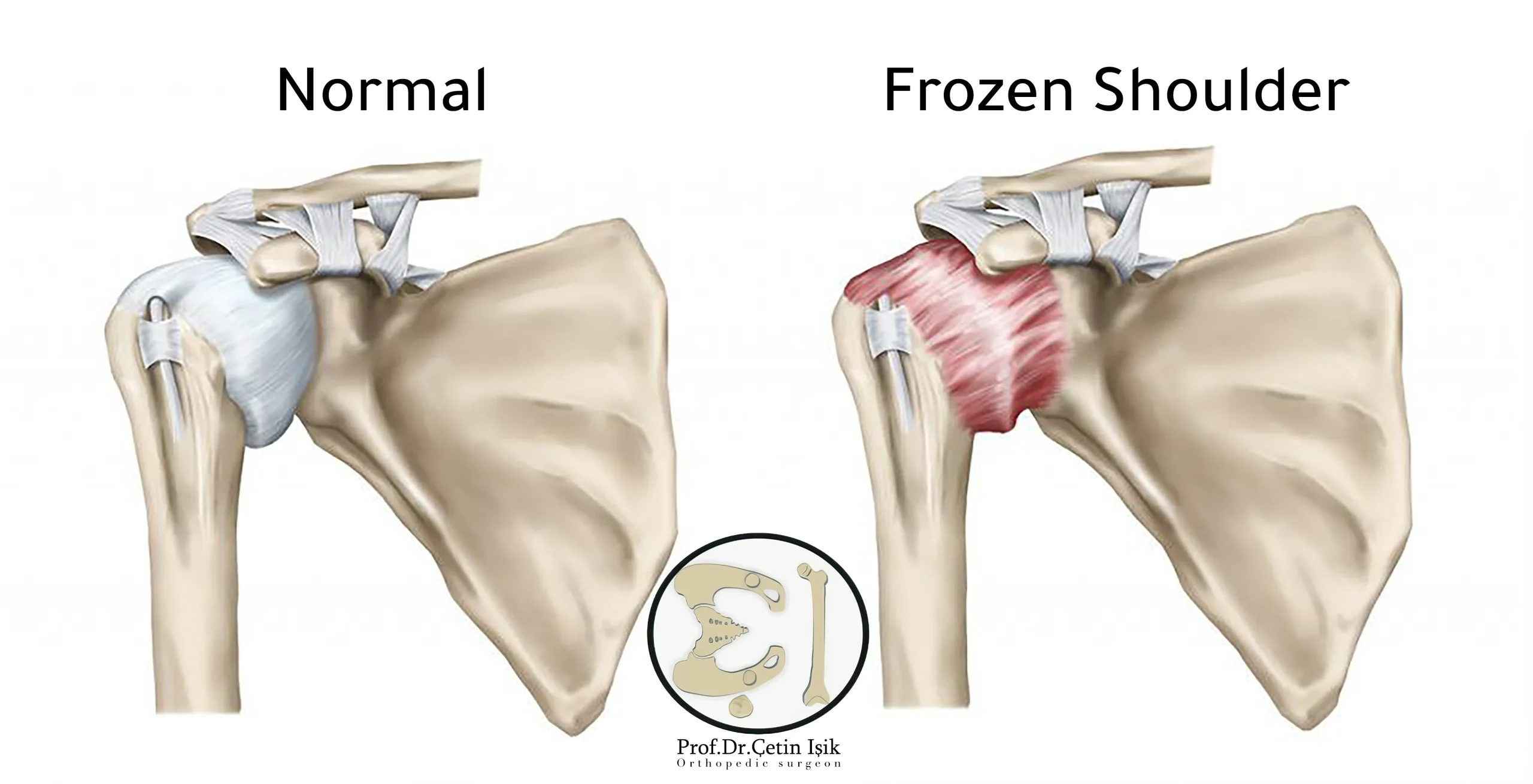
The joint is completely surrounded by a connective tissue called the shoulder capsule, which secretes synovial fluid, which allows the joint to move without friction.
Frozen shoulder disease known as frozen shoulder Adhesive capsulitis Adhesive capsulitis is a painful condition that occurs when the joint capsule thickens as a result of the formation of scar tissue in it, which makes joint movement limited and stiff.
Frozen shoulder usually affects people between the ages of 50 and 60 years, and women in general are more susceptible to frozen shoulder than men, and the estimated incidence of the disease among individuals is about 3%.
Risk factors for frozen shoulder disease
There are several common factors that increase the incidence of frozen shoulder, and they are:
- Age: As the incidence increases in adults after over 40 years.
- Gender: Women make up 70% patients with frozen shoulder.
- Recent injury: Surgery or a broken arm can cause immobility while the joint heals, which increases the rigidity of the capsule.
- Diabetes: As 10-20% patients with diabetes suffer from frozen shoulder, their symptoms may be more severe.
There are other health problems that increase the possibility of developing frozen shoulder disease:
- Brain attack
- Hyperthyroidism
- Hypothyroidism
- Heart diseases and vascular diseases
- Parkinson's disease
- Dupuytren's contracture
- Cancer
- Tuberculosis
Causes of frozen shoulder disease
Doctors do not yet know a primary cause for the development of frozen shoulder. It is believed that it may be caused by... Shoulder Arthritis And the surrounding capsule or an injury to the shoulder, such as an injury to the rotator cuff (muscles and tendons of the shoulder).
Frozen shoulder symptoms
The most obvious symptom of frozen shoulder is mild to moderate pain in the shoulder and muscles around the upper arm with shoulder joint stiffness.
Symptoms are usually categorized into three stages, as the symptoms of frozen shoulder gradually worsen over time, and the signs can disappear within two to three years.
- The first stage: It is called the freezing stage, in which the pain develops gradually and gets worse at night, as the joint moves with difficulty. This stage can last from 6 to 9 weeks.
- The second phase: It is the frozen shoulder stage, where the pain does not worsen, yet the shoulder remains stiff and movement is restricted. It lasts from 4 to 6 months.
- The third level: Or the dissolution stage is characterized by a relative ease of movement and may eventually return to normal. The pain may fade, but it appears sometimes in a episodic form. This takes between 6 months and up to two years.
Diagnosis of frozen shoulder
To diagnose frozen shoulder, the doctor performs both a physical examination and x-rays after taking the medical history, history of injury and onset of pain, and also asking the patient about his health history, occupation, and daily activity.
physical examination
The doctor evaluates the mobility of the shoulder and arm, and if there is a limitation in the natural range of the joint, through a set of physical tests that include:
Gently moving the arm in different positions by the doctor (negative movement), then asking the patient to do the same (positive movement).
The movement most often affected in frozen shoulder disease is passive external rotation.
radiography
X-rays may be taken to rule out other conditions. Advanced imaging tests such as MRI are usually not needed.
Frozen shoulder treatment
In most cases, frozen shoulder gets better on its own, but due to the slow course of the disease, recovery may also take several years to complete.
The goal of any treatment is to reduce pain, control arthritis and increase shoulder mobility, and to get the best results, it is preferable to start the appropriate treatment quickly.
The doctor first recommends conservative measures to treat frozen shoulder disease, depending on the age and severity of the injury, which includes the following:
Hot or cold compresses: Apply to the joint several times a day to reduce mild joint pain.
Medications: Over-the-counter or non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, help relieve shoulder pain and control shoulder inflammation.
Physiotherapy and exercise: Physical therapy is useful in improving the range of motion of the joint, as well as practicing exercises that include passive stretching of the external rotation of the joint. It is preferable to follow the instructions of the physical therapist to avoid wrong movements.
Hydrodilatation (dilation of the joints): It is a procedure in which a large amount of sterile fluid is injected into the shoulder joint to widen and stretch the shoulder joint capsule, thereby improving mobility.

TEN: Transcutaneous electrical nerve stimulation. It is a therapeutic method that uses low-voltage electrical currents to help relieve pain Shoulder pain Frozen, these pulses are delivered by a small battery-operated device through electrodes placed on the skin of the affected joint.
Steroid injection: Steroids are injected by the doctor directly into the shoulder joint to relieve joint inflammation and severe swelling, and it is not recommended to repeat injections to avoid long-term side effects.
Surgical treatment of frozen shoulder disease
If nonsurgical treatments don't work after a few months, your doctor may recommend:
Shoulder maneuver: The patient is under general anesthesia while the doctor manipulates the shoulder, which involves stretching or even tearing the capsular tissue to release the stricture and increase range of motion.
Shoulder arthroscopy: In it, incisions are made around the shoulder joint, allowing the surgeon to insert small surgical tools and cut out the scar tissue. This is called a capsular release.
In the case of undergoing surgery, the recovery time may vary from 6 weeks to 3 months, with the importance of physical therapy accompanying this stage, and the long-term results are well satisfactory.
Complications of frozen shoulder disease
Complications of frozen shoulder include:
- Persistent pain and stiffness: Shoulder pain may persist in some patients for up to 3 years, even after surgery.
- Bone and soft tissue damage: Shoulder maneuvers can sometimes fracture the humerus or tear the biceps or subscapularis tendon.
- Recurring frozen shoulder: While it is rare, it is possible for frozen shoulder to return and this condition is more common if it is associated with chronic diseases such as diabetes.
Prevention of frozen shoulder disease
These tips may help prevent the development of frozen shoulder:
- Maintain the mobility of the shoulder joint as much as possible.
- In the event of shoulder pain or joint stiffness It must be treated early.
- when undergoing surgery or injury in the shoulder area; The patient must adhere to the doctor's instructions and follow up with a physical therapist to move the shoulder safely so that he can return to the usual activities of life.
Sources:
Common questions
A stiff shoulder is a common condition and its main symptoms include: pain, stiffness and limitation in the normal range of motion.
Mobility impairments can be serious and tend to get worse over time, so they should be treated as soon as symptoms begin.
Supervised physiotherapy usually lasts from 1 to 6 weeks, in addition to home exercises and stretching that have a positive impact throughout the recovery period.
Treatment measures for frozen shoulder vary, such as: taking painkillers, steroid injections into the joint, physical therapy, and finally surgery as a last resort.




