Laser beam offers a new way to treat bone cancer
Of the many methods of treating cancer, surgery is the oldest and most successful in treating cancer. Even with the advent of chemotherapy, radiotherapy and many experimental therapies such as bacteria seeking to destroy cancer cells, cancers, for the most part, simply need to be eradicated from the patient's body.
The goal is to remove all of the cancerous tissue while preserving as much of the surrounding healthy tissue as possible.
But because it is difficult to draw a clear line between cancerous tissue and healthy tissue, surgeons often remove more healthy tissue than is necessary for fear that some cancerous cells may remain in the extremities.
This is normal in many tissues, but when a patient has BBone cancer This causes a big problem. Bone presents a unique challenge during surgery because it is difficult to compare with other tissues because it grows much more slowly than other types of tissue.
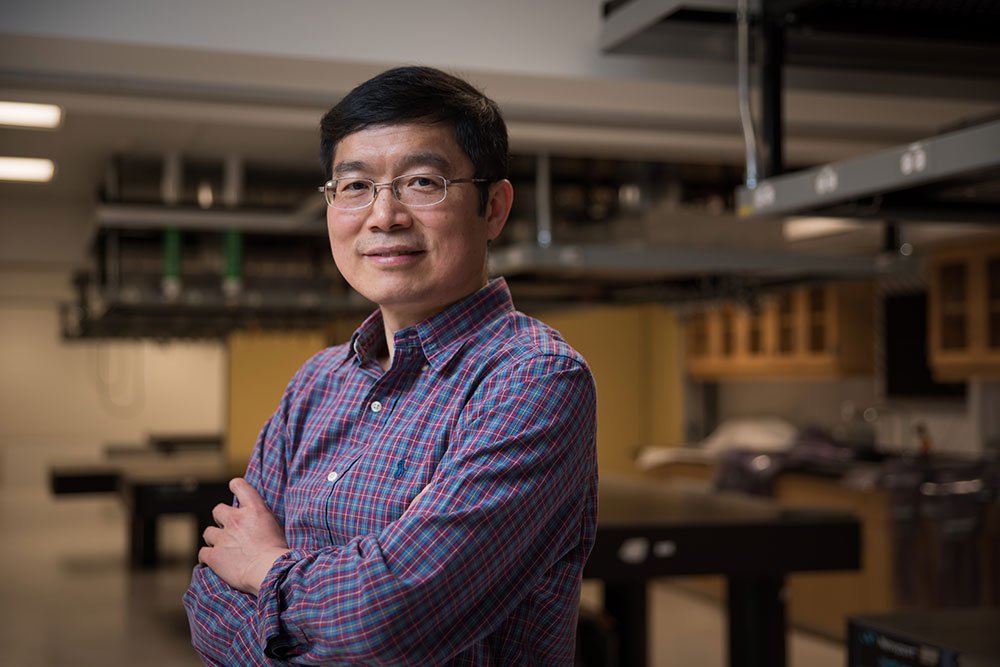
“It is very difficult for bone to grow, so if you remove a part of the bone, you lose it completely,” says Lihong Wang, a professor of medical engineering and electrical engineering.
A new discovery in bone and joint cancer surgery
New diagnostic imaging technology developed by researchers at Caltech gives surgeons the ability to make cuts dozens of times more precise than conventional methods, allowing them to preserve up to 1,000 times more healthy tissue and giving patients an easier recovery.
Conventional methods take a long time to determine if a bone slide contains cancerous cells.
First the cancerous mass is removed from the bone along with the healthy tissue and sent to a laboratory where the solid calcium matrix is slowly dissolved, leaving only the living cells behind.
The remaining material from the living tissue is then sliced and analyzed.
Because the operation can take anywhere between one and seven days to complete, surgeons cannot rely on it during surgery to determine the integrity of the tissue around the cancerous mass, and so they remove more healthy tissue than would be necessary—more than if it were in the soft tissue that They can be biopsied quickly.
The new imaging technology, called 3D ultraviolet light scanning photoacoustic microscopy, or UV-PAM, aims to replace the traditional method for identifying cancerous bone tissue.
Because the procedure takes only minutes, it provides the surgeon with the ability to differentiate between healthy bone tissue and cancerous bone tissue during surgery.
Like other photoacoustic imaging technologies developed by Professor Wang, UV-PAM works by using laser light to cause molecules to vibrate in living tissue.
These vibrations occur at ultrasound frequencies and can be used to image tissues and organs in the same way that ultrasound is used to image a fetus.
UV-PAM uses laser-tuned ultraviolet waves to cause DNA and RNA molecules to vibrate.
Because cancer cells have a different structure, and they contain much more DNA than healthy cells, the area of cancerous tissue absorbs more UV light, and thus will provide a stronger ultrasound signal than healthy tissue, making it clearer for the patient to identify the malignant tissue that needs to be removed. to the surgeon.
“We can provide results in 11 minutes, so they know exactly where to cut,” says Wang.
"We just provide the images to the pathologists," says Professor Wang. “That is, they use the same old patterns of recognition to determine what is cancerous and what is healthy. This is their training."
At the moment, the technology is only used in a laboratory environment. Dr. Wang says he hopes to bring it into the real world where it can be used on patients directly, but first he plans to make some improvements to the device.
“We would like to give it a finer spatial resolution and faster imaging speed so we can see some of the details inside the cell nucleus more quickly,” he says. Can we bypass standard pathology? We are working on it.”
paper describing UV-PAM , titled “Intraoperative Label-Free Bone Histology with Deep Learning-Assisted Ultraviolet-Selection Microscopy,” appeared Sept. 19 in the journal Nature Biomedical Engineering.