ما هو التهاب المفاصل الروماتويدي؟
التهاب المفاصل الروماتويدي (Rheumatoid Arthritis) هو مرض مناعي مزمن يهاجم فيه الجهاز المناعي المفاصل، مما يؤدي إلى التهاب مزمن وألم وتورم يمكن أن يؤدي إلى تلف المفصل إذا لم يتم علاجه بشكل فعال. يصيب هذا المرض النساء أكثر من الرجال، وعادةً ما يبدأ بين سن 30 و60.
Symptoms of rheumatoid arthritis
| العرض | التوضيح |
|---|---|
| Joint pain | خاصة في الصباح أو بعد فترة من الراحة |
| تيبّس المفاصل | غالبًا في الصباح ويستمر لأكثر من 30 دقيقة |
| تورم واحمرار | حول المفاصل المصابة |
| الإرهاق العام | الشعور بالتعب المستمر |
| الحمى وفقدان الوزن | أحيانًا في المراحل المتقدمة |
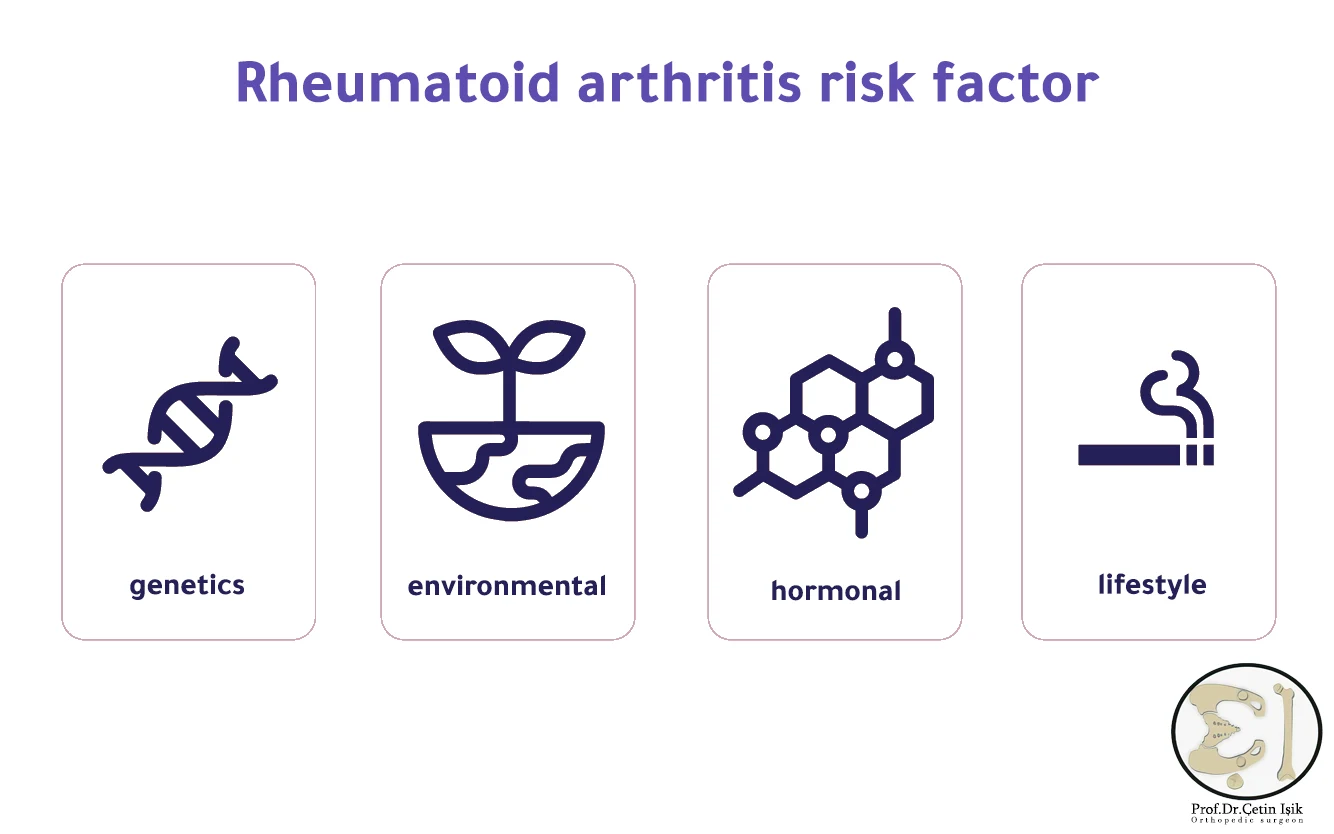
أسباب التهاب المفاصل الروماتويدي
السبب الدقيق غير معروف، ولكن هناك عوامل تساهم في ظهوره:
- heredity: وجود تاريخ عائلي يزيد من احتمال الإصابة.
- البيئة: التعرض لعدوى فيروسية أو بكتيرية قد يحفّز المرض.
- الهرمونات: خاصةً لدى النساء، حيث يزداد نشاط المرض مع تغيرات هرمونية.
- smoking: عامل خطر مؤكد لظهور وتفاقم المرض.
Diagnosis of rheumatoid arthritis
يُعتمد على مزيج من الفحوصات السريرية والمخبرية:
- Clinical examination: تقييم عدد المفاصل المؤلمة والمتورمة.
- Blood tests:
- العامل الروماتويدي (RF)
- الأجسام المضادة CCP
- معدل ترسيب كريات الدم الحمراء (ESR)
- بروتين C التفاعلي (CRP)
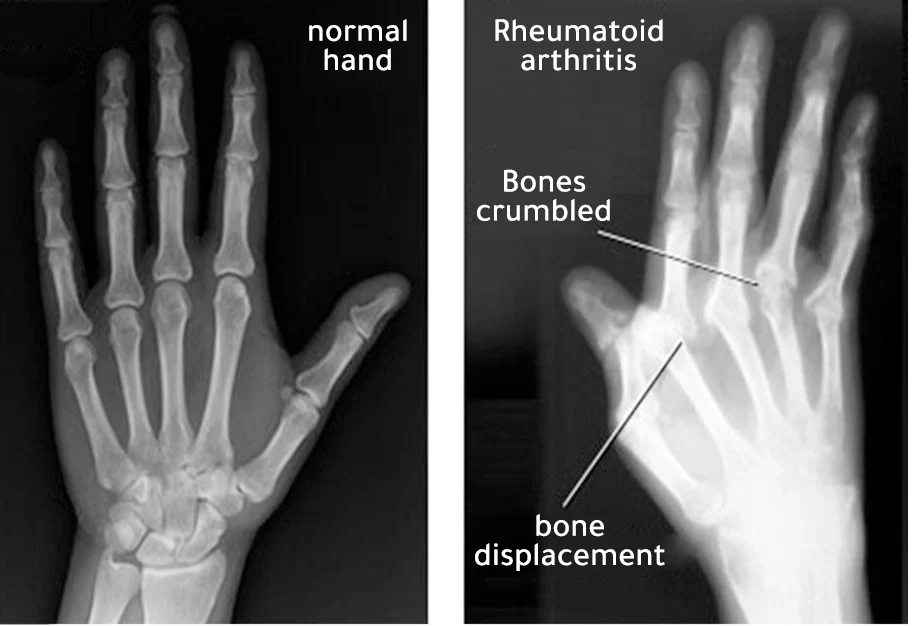
- الأشعة: للكشف عن تلف المفاصل (أشعة سينية، رنين مغناطيسي).
Rheumatoid arthritis treatment
أولاً: الأدوية
| نوع الدواء | أمثلة | الفائدة |
|---|---|---|
| مضادات الالتهاب غير الستيرويدية (NSAIDs) | ايبوبروفين، ديكلوفيناك | تقليل الألم والالتهاب |
| الكورتيكوستيرويدات | بريدنيزولون | تقليل الالتهاب بشكل سريع |
| الأدوية المُعدِّلة للمرض (DMARDs) | ميثوتريكسات، هيدروكسي كلوروكين | تبطئ تقدم المرض |
| الأدوية البيولوجية | إيتانيرسيبت، أداليموماب | تستهدف الجهاز المناعي بدقة أعلى |
💡 ملاحظة: يتم اختيار الدواء المناسب بحسب حالة المريض ومدى نشاط المرض، وتُراقب الجرعات بدقة لتفادي الآثار الجانبية.
ثانياً: العلاج الطبيعي والوظيفي
- تمارين خفيفة لتحسين مرونة المفاصل.
- جلسات علاج طبيعي لتقوية العضلات الداعمة.
- استخدام أجهزة داعمة لتقليل الضغط على المفاصل (مثل الجبائر والمعصمات).
ثالثاً: التغيير في نمط الحياة
- Quit Smoking
- اتباع نظام غذائي مضاد للالتهابات: غني بالخضروات، زيت الزيتون، الأسماك الدهنية.
- Maintain a healthy weight لتقليل الضغط على المفاصل.
- الحصول على قسط كافٍ من النوم
رابعاً: الجراحة
في الحالات المتقدمة قد يُوصى بالتدخل الجراحي:
| نوع الجراحة | الهدف |
|---|---|
| Joint replacement | عند تآكل المفصل بالكامل |
| تنظيف المفصل بالمنظار | إزالة الأنسجة الملتهبة |
| دمج المفاصل | لتثبيت المفاصل غير المستقرة |
هل يمكن الشفاء من التهاب المفاصل الروماتويدي؟
لا يوجد حاليًا علاج نهائي، لكن العلاجات الحديثة فعالة في السيطرة على الأعراض وإبطاء تقدم المرض، مما يسمح للمريض بحياة طبيعية إلى حد كبير.
نصائح للوقاية من نوبات الالتهاب
- الالتزام بالعلاج بشكل منتظم
- مراجعة الطبيب دوريًا لتقييم فعالية الدواء
- تقليل التوتر النفسي
- ممارسة الرياضة الخفيفة بانتظام
الأسئلة الشائعة حول التهاب المفاصل الروماتويدي
هل هو مرض وراثي؟
لا يُعد وراثيًا بشكل مباشر، لكنه أكثر شيوعًا في العائلات التي يوجد بها حالات إصابة.
هل يصيب الأطفال؟
نعم، يوجد نوع خاص يُعرف باسم “التهاب المفاصل الروماتويدي الشبابي (JRA)”.
هل يمكن الحمل أثناء العلاج؟
بعض الأدوية غير آمنة أثناء الحمل، لذلك يجب استشارة الطبيب والتخطيط المسبق.
خلاصةعلاج التهاب المفاصل الروماتويدي يتطلب خطة متكاملة تشمل الأدوية، والعلاج الطبيعي، ونمط حياة صحي. الكشف المبكر والالتزام بالعلاج هما المفتاح لتفادي تلف المفاصل وضمان نوعية حياة أفضل للمريض.
Sources:
Common questions
Treatment of rheumatoid arthritis is based on relieving symptoms, and if medication is adhered to, results will be excellent, especially when using DMARDs, an acute inflammatory attack of 35% may occur if the medication is not taken for a year.
Blood tests are the basis for diagnosis because they detect the immune changes that will cause the disease before its symptoms worsen.
Stress, lack of sleep and psychological stress in addition to other diseases such as cold and flu.
Untreated rheumatoid arthritis can cause entire joints to become damaged and need to be replaced.
Unfortunately, the drug cannot be completely dispensed with because it is a chronic and progressive disease




