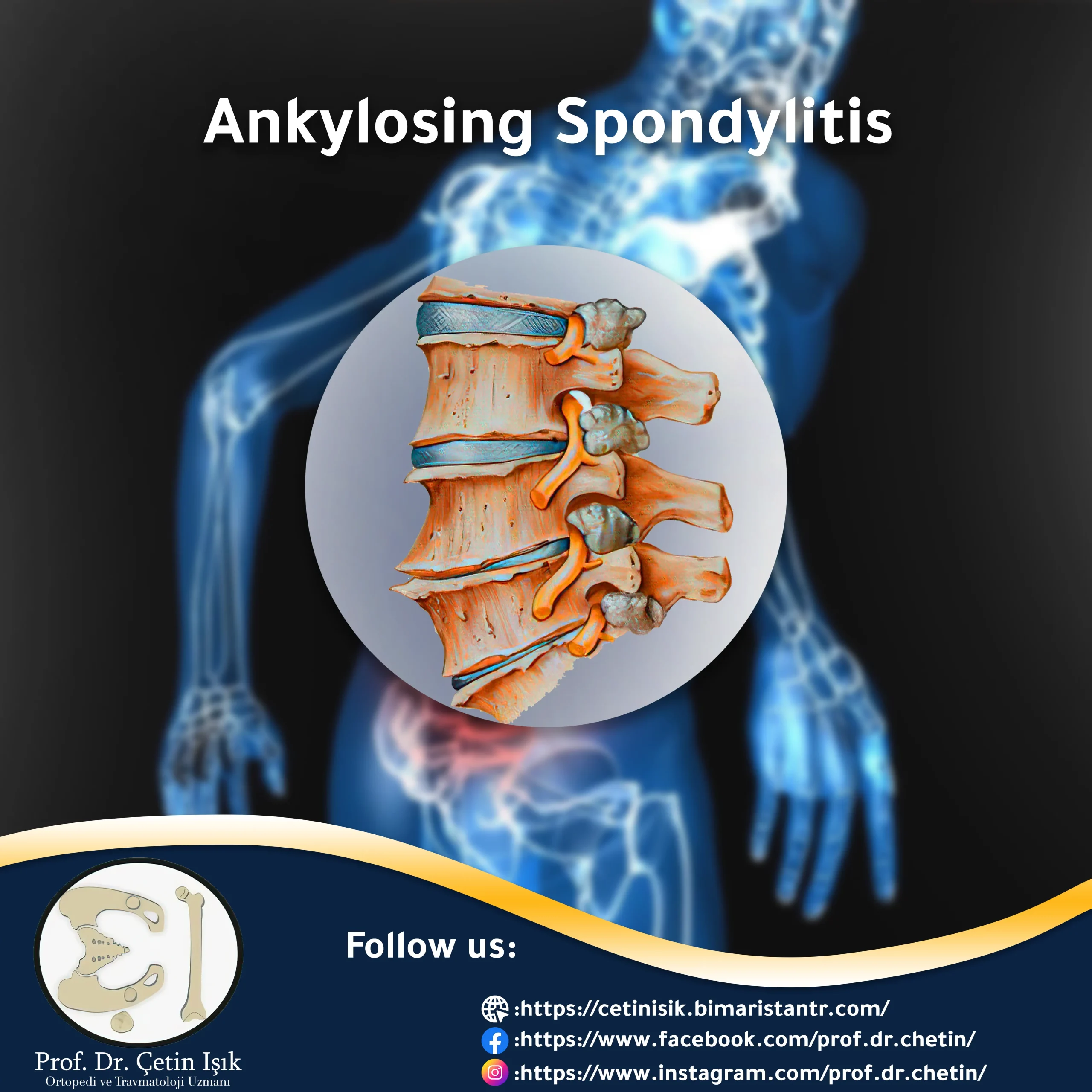
Ankylosing spondylitis is a rare form of arthritis that causes chronic pain and stiffness in the spine and peripheral joints, and requires early treatment to prevent deformities from developing over time.
What is ankylosing spondylitis?
Ankylosing spondylitis, or ankylosing spondylitis, is a chronic inflammatory disease, a form of arthritis that primarily affects the spine, in which ligaments and tendons attach to the bones of the spine and even the bones of the peripheral joints. As a result of the inflammatory process, new bone is formed in the spine, leading to bone fusion, then the spine stiffens, its flexibility decreases, and in advanced cases, it causes deformation.
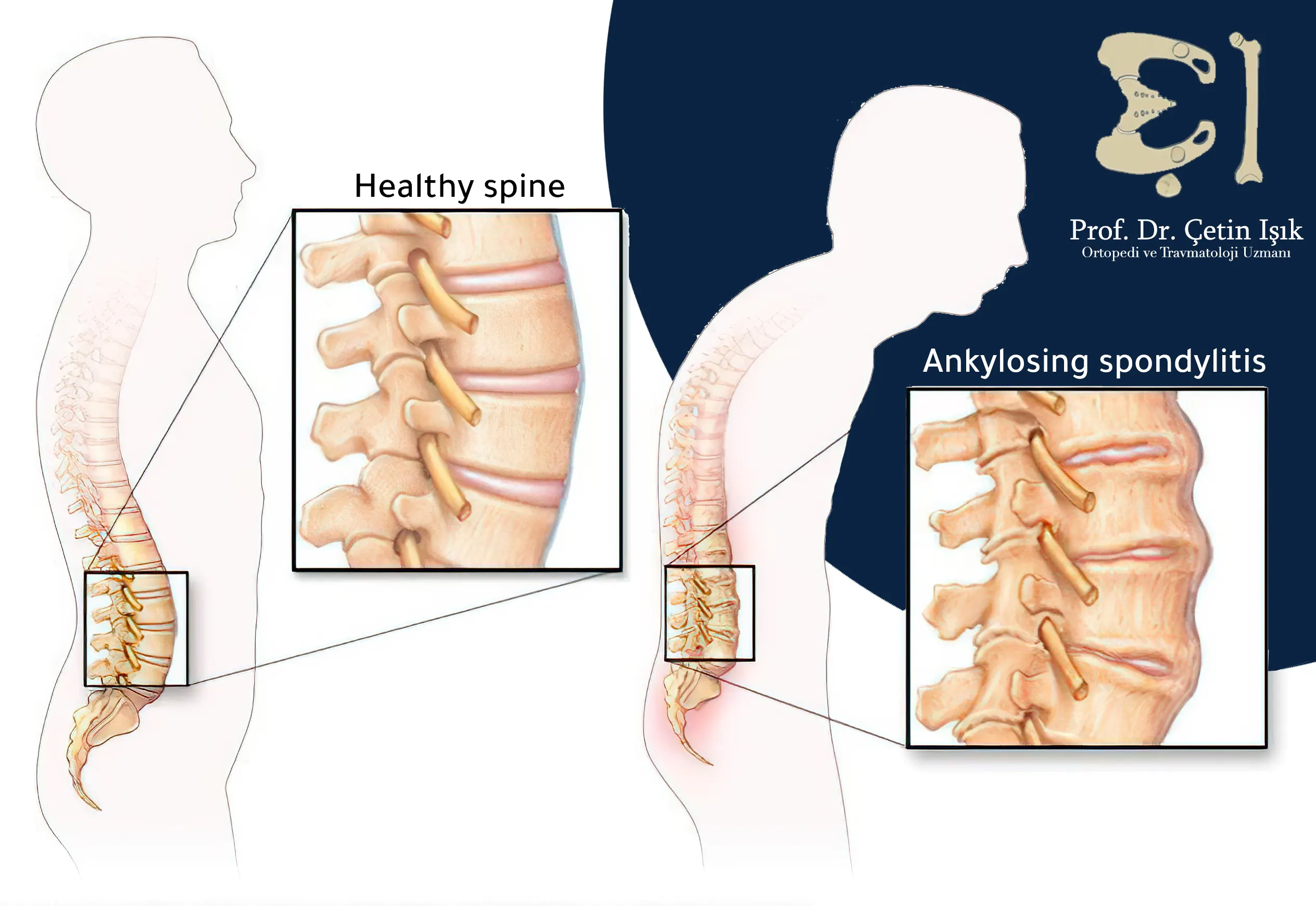
Ankylosing spondylitis often develops in the lower back when the spine and iliac joints are attached, and may affect other parts of the spine, causing problems such as severe kyphosis.
Types of ankylosing spondylitis
Some experts have classified ankylosing spondylitis according to the location of the injury and the radiographic findings as follows:
- Axial ankylosing spondylitis: Inflammation is located in the axial skeleton (spine) and has typical radiographic findings of the sacroiliac joint.
- Non-radiographic ankylosing spondylitisClinically similar to axial spondylitis, but without radiographic findings on x-rays of the sacroiliac joint of the spine.
- Peripheral ankylosing spondylitis: Where the inflammation is located in the peripheral joints of the body and spares the spine.
Risk factors for ankylosing spondylitis
Anyone can develop ankylosing spondylitis, however some factors may increase the risk of developing it, including:
- Family history and genetics: Ankylosing spondylitis is more common among first-degree relatives of the patient.
- Race: An increased prevalence of disease has been observed in the black race.
- Age: Unlike arthritis and other rheumatic diseases, the disease usually begins to appear gradually between the ages of 20 and 40, and symptoms may appear at an earlier age.
- Gender: Ankylosing spondylitis affects three times more men than women.
- Having certain diseases, such as ulcerative colitis, Crohn's disease and psoriasis, increases the risk.
Causes of ankylosing spondylitis
The cause of ankylosing spondylitis and the chronic inflammatory process in it is not yet known. However, researchers found an essential gene in most patients, HLA-B27. However, many people have this gene and do not have ankylosing spondylitis, which suggests the role of environmental factors such as bacterial infection. in making it too.
Symptoms of ankylosing spondylitis
Symptoms of ankylosing spondylitis vary greatly from person to person. Some people have mild episodes of pain that come and go, and others have severe chronic pain.
Symptoms of ankylosing spondylitis, whether they are mild or severe, are exacerbated by an inflammatory attack and improve during the period of remission. Another distinguishing feature is the improvement of pain when moving and exercising, and the pain increases when sitting and in the morning period.
Since the disease can affect different areas of the body other than the spine, a patient may have various symptoms, which include:
- Pain and stiffness in a number of other joints in the body, such as pain andNeck stiffnessShoulder, hip, knees and feet
- Difficulty breathing deeply if the rib joints are affected
- Osteoporosis
- Loss of appetite and weight loss
- Rash
- Abdominal pain and itching.
- Extreme tiredness
- Vision changes and eye pain due to uveitis
Diagnosis of ankylosing spondylitis
It often takes years for ankylosing spondylitis to be properly diagnosed, due to the progressive development of the disease and the slow onset of symptoms with other suspected conditions.
However, early diagnosis is crucial for obtaining appropriate treatment and preventing worsening of the health condition and the occurrence of bone deformities.
First, the doctor takes the medical history by inquiring about the symptoms, health and family history of the patient, and then performs a physical examination, which includes examining the joints of the body, monitoring movement and flexibility by conducting some simple tests, and making sure to take a deep breath to check for stiffness and inflammation of the ribs.
To help confirm the diagnosis of ankylosing spondylitis, the doctor will order laboratory and radiological tests:
Blood tests: Currently, there is no single test that diagnoses ankylosing spondylitis, but a blood test can be ordered to detect the HLA-B27 gene, which is present in the majority of patients.
Radiography:
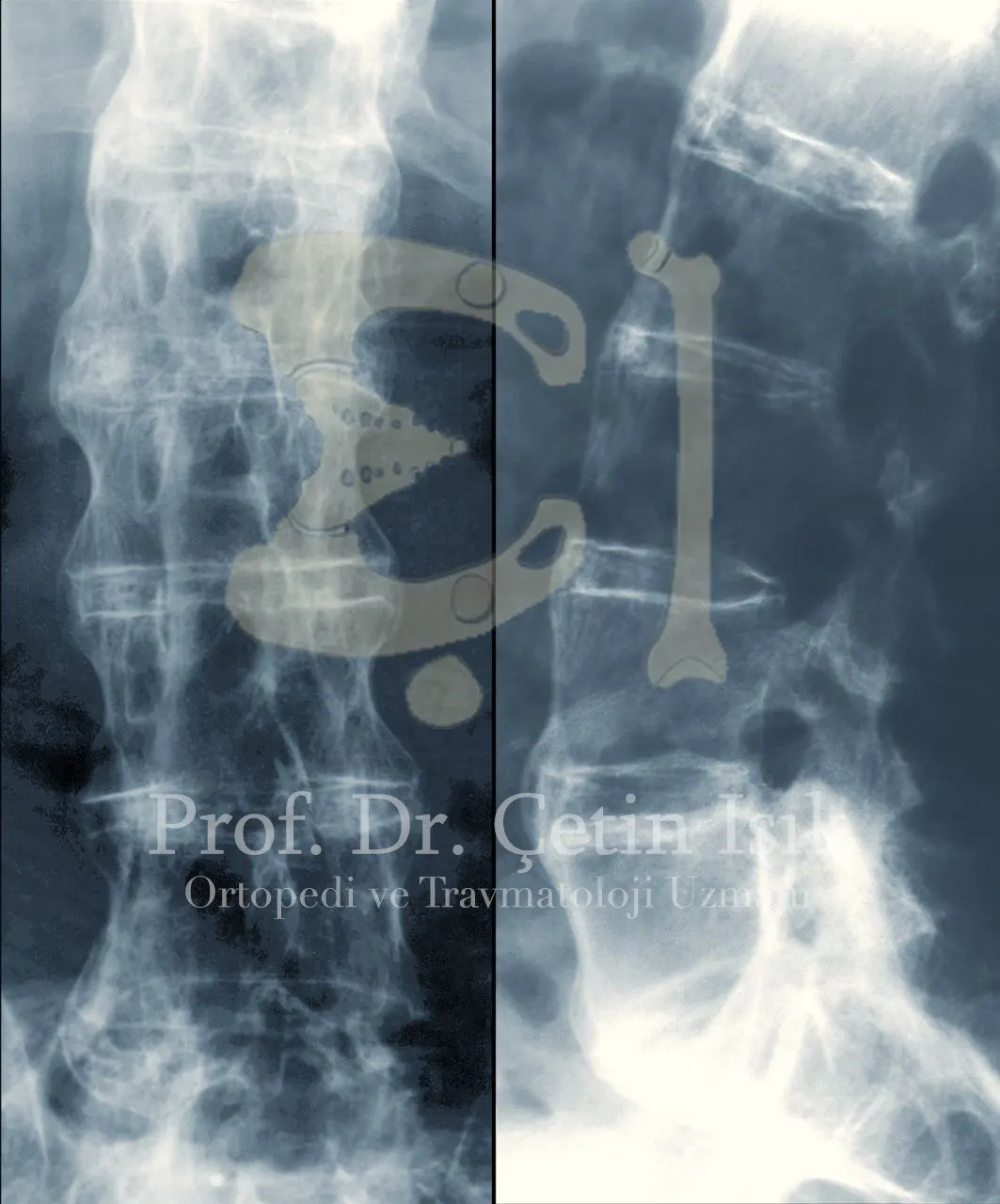
- X-ray: Which helps to see changes in the spine and peripheral joints, but in somewhat advanced stages of the disease, is used to monitor the progression of the disease and exclude other causes of joint pain and not in early diagnosis.
- Magnetic resonance imaging (MRI): It is the most sensitive, used in the diagnosis of ankylosing spondylitis in its early stages, as it detects arthritis before major changes in the bone occur.
Complications of ankylosing spondylitis
Because ankylosing spondylitis is a systemic immune disease; Its effect extends beyond the spine to affect many places in the body, and in the event of delay in treating ankylosing spondylitis for a long time, the following complications may appear:
- Fusion of the vertebrae
- Curvature of the spine
- Osteoporosis
- Uveitis and sensitivity to light
- Heart problems such as: aortic arteritis, arrhythmia and cardiomyopathy
- Jaw osteitis
- Cauda equina syndrome in lumbar spine injury
Ankylosing spondylitis treatment
There is no cure for ankylosing spondylitis, as it is a chronic disease whose symptoms continue to appear for life in the form of episodic or persistent, but the goal of treating ankylosing spondylitis is to relieve pain and control arthritis while maintaining its range of motion and preventing the development of complications.
The treatment options for the disease are varied, including:
Treating ankylosing spondylitis with medication
NSAIDs: Including naproxen and ibuprofen that relieve pain and inflammation.
Disease-modifying antirheumatic drugs (DMARDs): These include sulfalazine (Azulfidine) and methotrexate. This class of medications is prescribed to reduce joint pain and swelling.
Biological treatment of ankylosing spondylitis:
Modern genetically modified drugs help treat lesions caused by inflammatory bowel disease by altering the immune system, which include medicinal preparations such as:
- Interleukin IL-17 inhibitors.
- JAK kinase inhibitors.
- TNF inhibitors: These are the first of a group of biological drugs that work by preventing inflammatory chemical inducers called cytokines from being released in the body.
Five TNF inhibitors have been approved by the FDA:
- Adalimumab
- Certolizumab
- Etanercept
- Infliximab
- Golemwab
The problem with treating ankylosing spondylitis with biologic medications is that they increase the risk of infection by suppressing the body's immune system.
Ankylosing spondylitis treatment by injection
Corticosteroids are injected by the doctor and guided by ultrasound around the joints to relieve arthritis and temporarily relieve pain.
Herbal treatment of ankylosing spondylitis: Many natural herbs are considered to help relieve joint pain without annoying side effects, such as ginger, turmeric, and willow tea.
Physical therapy and exercise
Physical therapy and exercise can help treat ankylosing spondylitis and prevent limited spinal motion and joint stiffness.
The physical therapist supervises the patient by designing a customized program that helps the person maintain the mobility of the vertebrae and joints and in good posture.
An ideal exercise program should include the following four components:
- Stretching exercises: To increase flexibility, prevent muscle stiffness, and reduce the risk of fusion.
- Aerobic exercises: Which raises the heart rate and improves blood circulation in the body and lung functions, such as swimming and walking.
- Muscle exercise: To strengthen the back muscles, which supports the spine.
- Balance exercises: To improve stability and reduce the risk of falls and fractures.
Surgical treatment of ankylosing spondylitis
Although most people with ankylosing spondylitis can be treated without surgery, a surgical option may be necessary in certain cases. The surgeon chooses the type of procedure the patient needs based on the disease's symptoms, age, and general health.
Among the surgical options are:
Laminectomy: In the event of compression of the nerves or spinal cord and feeling pain, numbness or tingling, this operation helps relieve the pressure caused by removing the back arch of the vertebrae
Osteotomy: In cases of severe kyphosis, which greatly hinders the patient's life, the bones are cut and reshaped to improve posture and movement, a rare process in cases of ankylosing spondylitis.
Spinal fixation and fusion: People with ankylosing spondylitis have a higher risk of spinal fractures, which are often unstable, and the surgeon must repair them surgically because they are threatening the spinal cord.
Read more about: Lumbar spine fixation surgery to straighten the back.
Joint replacement: Such as the shoulder, knee and hip joints, may be necessary after years of treatment in the event of severe damage.
In the event of an inquiry about ankylosing spondylitis and its treatment, you can Contact us to answer it.
Living with ankylosing spondylitis
It is not easy to live with ankylosing spondylitis and its chronic pain, especially if it is left untreated.
Over time and the development of spondylitis, the patient needs to take steps that he can take to reduce the effects caused by it, and these are some of them:
- Quit Smoking: It reduces the effectiveness of treatment and worsens symptoms.
- Eating a healthy, integrated diet: By including vegetables, fruits, whole grains and proteins, and limiting alcohol, sugar and saturated fats, which helps control inflammation and maintain a healthy weight and it is important to controlling ankylosing spondylitis.
- Use of assistive devices: Such as crutches and orthoses if walking causes joint pain and difficulty in movement.
- Attention to mental and psychological health: Stress may increases in the patient as a result of unexpected attacks or chronic pain, it is important to practice some relaxation techniques such as yoga or meditation and deep breathing to make living with spondylitis easier.
Sources:
Common questions
Patients with ankylosing spondylitis can usually control the disease, and if treatment is not started early, it can cause severe disability due to the fusion of the bones in the spine in a fixed position, and damage to other joints such as the thigh and knee.
There is no cure for ankylosing spondylitis, but the treatment options available can help relieve symptoms and reduce damage to the peripheral joints and spine.
Heredity can play an important role in the incidence of ankylosing spondylosis, as the incidence of people from one family is higher, and the probability of passing the HLA-B27 gene by 50% from father to children supports this.