The treatment of osteomyelitis involves a combined effort between medical and surgical disciplines, the two main aspects of treatment being surgical containment of the infection and prolonged antibiotics.
What is osteomyelitis?
Osteomyelitis is a bone infection affecting the long bones, caused by a bacterial or fungal infection of the bloodstream or surrounding tissues, causing painful swelling of the bone marrow and the soft tissues within the bones.
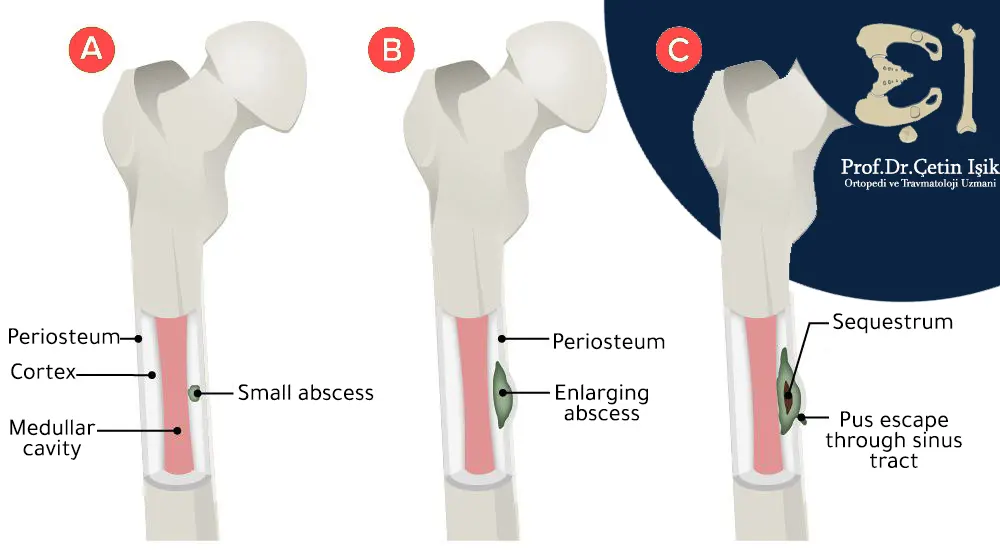
Osteomyelitis causes occlusion of blood vessels in the affected bone, and consequently, perfusion and necrosis, and the spread of infection locally, through the bony cortex or under the periosteum, with the formation of skin abscesses that may drain through the skin automatically.
Osteomyelitis is one of the oldest recorded diseases, affecting about 2 to 5 out of every 10,000 people.
Infection can occur at any age, and infections of long bones such as the bones of the legs or arms are most common in children, especially those under the age of 3 years.
But the risk of infection can increase with age, as older people face a number of health problems such as diabetes and orthopedic surgery that increase the risk of infection and inflammation in the spine.
Causes of osteomyelitis
Osteomyelitis results in different ways;
Spread from infected adjacent tissue, a contaminated artificial joint, or open wounds (contaminated fractures or in orthopedic surgery):
make up About 80% cases of osteomyelitis, which is often polymicrobial, the most important one is Staphylococcus aureus which presents in 50% patients, and also common bacteria are Streptococcus and anaerobes.
It often affects the feet, such as diabetic patients, or in the sites adjacent to pressure ulcers such as the pelvic bones, as well as in the sites where the bone has penetrated during surgery and fractures.
Diffusion through the bloodstream:
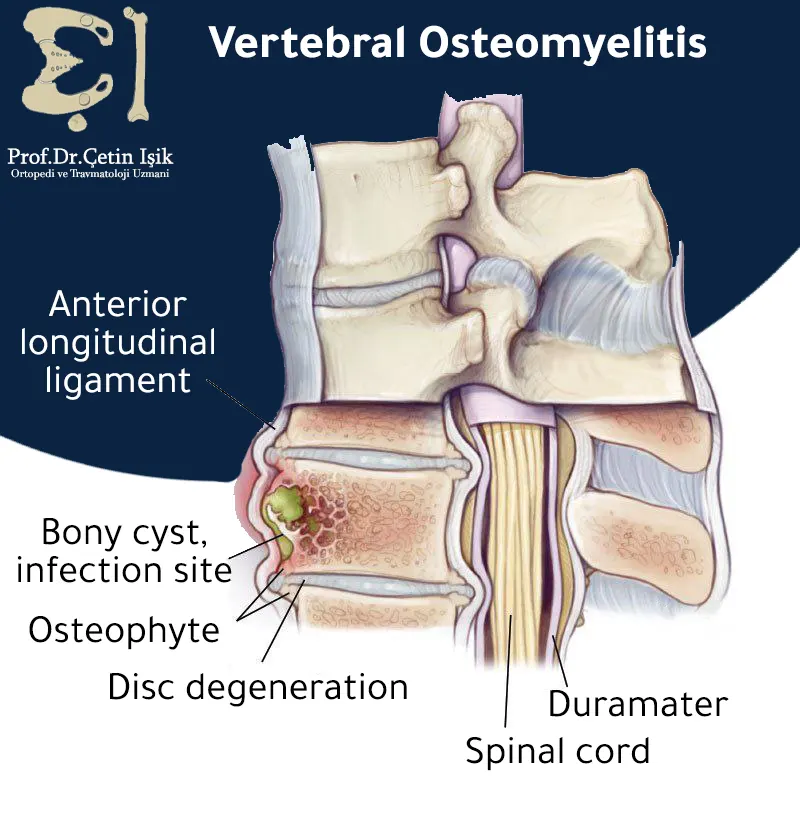
It is more common in children, and is caused by a single bacterial type that affects femur or humerus in children, and the vertebrae in adults.
The condition that affects the vertebrae is called Vertebral osteomyelitis Which especially affects the elderly or those who undergo dialysis sessions or use non-sterile needles to inject drugs, causing chronic back pain that worsens with movement and treatments such as rest, heating and analgesics are ineffective.
Direct spread (invasion):
Bacteria and fungi can be transmitted directly to bone through open fractures, during bone surgery, or using contaminated equipment.
Risk factors for osteomyelitis
Many risk factors make the natural ability to fight infections in the body weak, such as:
- aging
- The presence of an artificial joint, as a result Hip replacement or the knee.
- Blood infections or sickle cell anemia.
- Diabetes, especially associated foot ulcers.
- Metal implants in bones, such as nails and plates.
- Pressure injuries (ulcers).
- Orthopedic surgeries, and recent fractures.
- Previous osteomyelitis.
- Weakened immune system, due to chemotherapy or another immune disease.
- Drug abuse and use of contaminated needles.
- Cases requiring a catheter or intravenous tube.
Types of osteomyelitis
Choosing the best method for treating osteomyelitis depends on the severity of the infection, and is classified into:
- Acute osteomyelitis: This type usually develops rapidly after two weeks of bone infection, and is characterized by inflammatory changes in the bones, inflammation in children tends to be acute, and delay in treatment can lead to developmental disturbances, deformity and life-threatening complications.
- Chronic osteomyelitis: In the case of poor treatment of acute osteomyelitis, it develops into the chronic form after six weeks of infection, and is characterized by the presence of necrosis of the bone, destruction of the structure and the formation of granules in it, and it may not show any symptoms for months or years.
Symptoms of osteomyelitis
Symptoms of osteomyelitis vary according to the type, cause, location and severity of the injury, and some people with chronic osteomyelitis may not have any symptoms.
The disease is characterized by pain accompanied by redness, high temperature and swelling in the area of the injury, in addition to this, there are other symptoms such as:
- Fever
- irritability or lethargy
- loss of appetite
- lower back pain
- Feeling sick and vomiting
- Sweating
- Drainage from an open wound
- Changes in walking, such as a limp
Diagnosis of osteomyelitis
The doctor first performs a physical examination for signs such as swelling, redness, and fever, and checks the patient's medical history, especially operations or accidents.
The patient is also asked to:
- Blood tests Such as: complete blood count (CBC), erythrocyte sedimentation rate (ESR), and c-reactive protein
- Radiographs: Such as X-rays, magnetic resonance imaging (MRI), and computed tomography (CT) scans to take pictures of the affected bone, spine, and surrounding muscles and joints.
- Orthopedic examination: It uses a small amount of safe radioactive materials to identify infections or fractures during the imaging examination.
- biopsy: A fine-needle biopsy is done to take samples of fluid from tissues and bones for examination and detection of the type of bacteria or fungi causing the infection to determine the appropriate treatment.
Osteomyelitis treatment in Turkey
Recovery from osteomyelitis can take a long time, and starting treatment with the first symptoms noticing within three to five days speed up the recovery process.
Treatment methods for osteomyelitis vary according to the cause and degree of infection, and treatment includes:
Antibiotic treatment: The use of antibiotics for long periods is the cornerstone of the treatment of osteomyelitis. The duration may last from four to eight weeks. Intravenous antibiotics are started in the hospital for one or two weeks and then taken orally.
Antifungal therapy: For fungal infections, treatment continues for several months if a fungal infection is suspected.
Needle aspiration: Doctors use it to drain fluid and pus if abscesses form.
Pain relievers (anti-inflammatories): To relieve the pain and treat inflammation.
Herbal treatment for osteoporosis: Although there are no natural herbs that specifically treat osteoarthritis, they do play a role in strengthening the immune system such as garlic, milk thistle, flaxseed, ginger, turmeric and basil.
Osteomyelitis surgery:
Surgical work is necessary for the patient in the treatment of osteomyelitis if:
- The infection lasted a very long time until the bone was eroded.
- Pressure in the inflamed area on nearby tissues such as the spinal cord.
- Accumulation of pus in the bones and abscess formation.
Prior to surgical intervention, it is important to reconstruct the vascularization of the limb, control diabetes and treat other host factors that may impede wound healing, including smoking, malnutrition, chronic hypoxia and immunodeficiency states.
If the infection damages the bone, we will need surgery called: debridement To remove the damaged part and dead tissue.
Debridement can leave an empty space in the bone, which is packed with an antiseptic bandage.

spine surgery: People with spinal osteomyelitis undergo this procedure to prevent the bones of the vertebrae from collapsing or putting pressure on the nerves and spinal cord.
Antibiotics are taken intravenously in the hospital after surgery as well.
In case you encounter any problem and go to the right medical advice for the treatment of osteomyelitis Contact with usDr. Çetin Işık will answer all your questions.
Complications of osteomyelitis
- Abscesses Abscesses can form when infection spreads to muscle and tissue, where pus drains from these pockets of pus through the skin. Patients with chronic osteomyelitis are more likely to have recurrent abscesses. Treating these abscesses with drainage may slightly increase the risk of skin cancer.
- Bone death: Also known as osteonecrosis, it can occur when swelling associated with an infection cuts off blood flow to the bones, and this is a rare condition, possibly leading to limb loss or amputation.
- Septic (bacterial) arthritis: Arthritis is caused by bacteria, and infection within the bones can sometimes spread to nearby joints.
- stunted growth: If osteomyelitis occurs in the very soft areas called growth plates at either end of the long bones of the arms and legs, the child's normal bones or joints can stop growing.
- Skin cancer: If osteomyelitis leads to an open sore that drains pus, the surrounding skin is at risk of developing squamous cell carcinoma.
Sources:
Common questions
Treatment of osteomyelitis takes from 4 to 6 weeks, and if the body infections are severe, it may reach up to 12 weeks, it is important to finish the treatment course of antibiotics even if the person feels better.
People with acute osteomyelitis are usually given penicillin, ampicillin or cephalosporins.
Yes, because it is an infection that requires immediate treatment for fear of complications. However, most bone infections go away when taking the prescribed antibiotics.