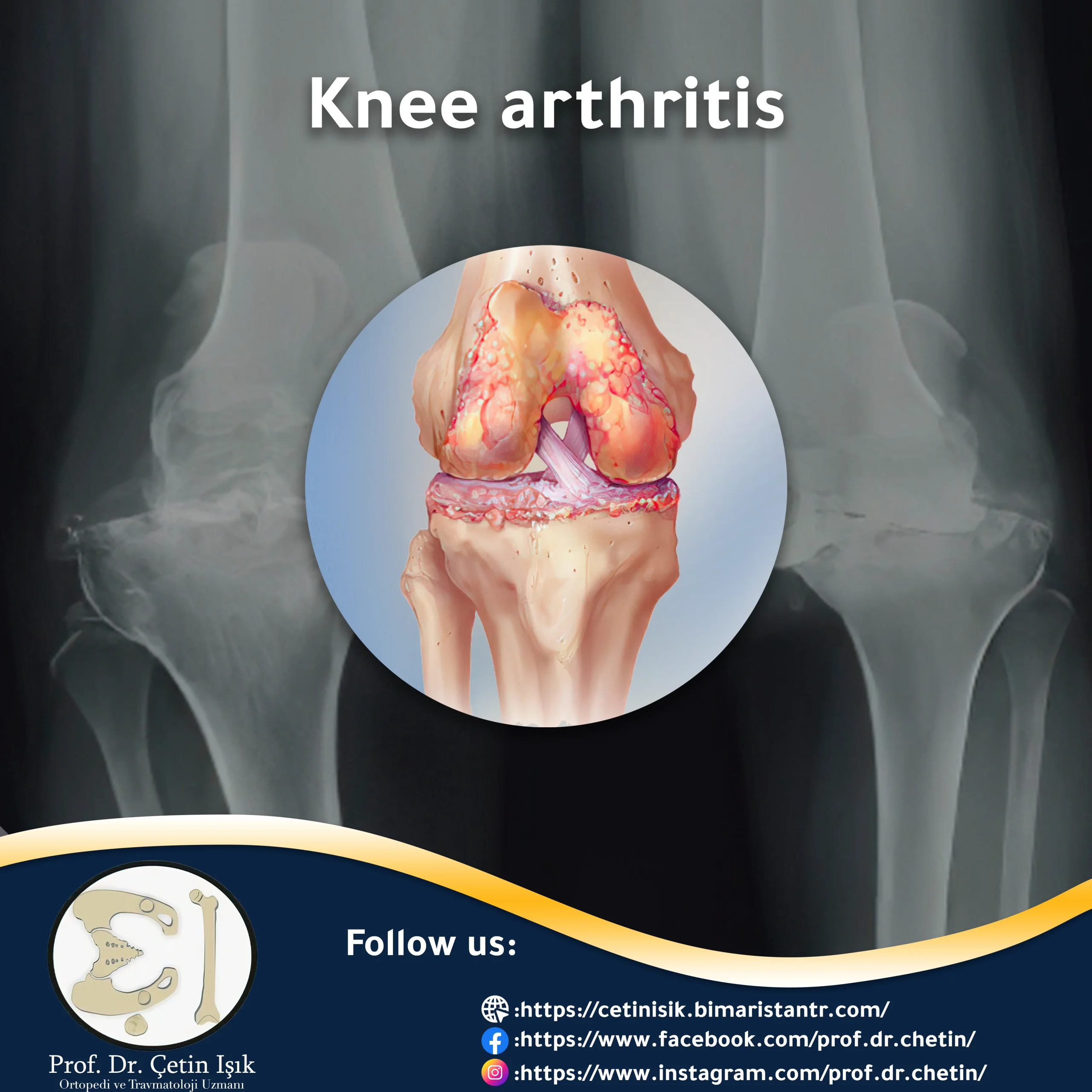
Knee arthritis is inflammation and deterioration of the joint cartilage. Pain, swelling, and stiffness are the main symptoms, but there are many treatment options available to relieve these symptoms.
Knee arthritis is a painful disease that gets worse with the passage of time and negatively affects the quality of life of patients, as it causes roughness of the joint surface, which leads to direct friction between the bones. Continue with us in this article to learn about knee arthritis, its most important types, causes, and available treatment methods to control its symptoms.
Knee arthritis
Knee arthritis occurs when the cartilage in the joint itself, which forms a slippery layer on the edges of the bones, acts as a cushion and allows the knee to bend and straighten smoothly, as cartilage damage causes constant pain and swelling in the joint while limiting the natural movement of the knee joint.
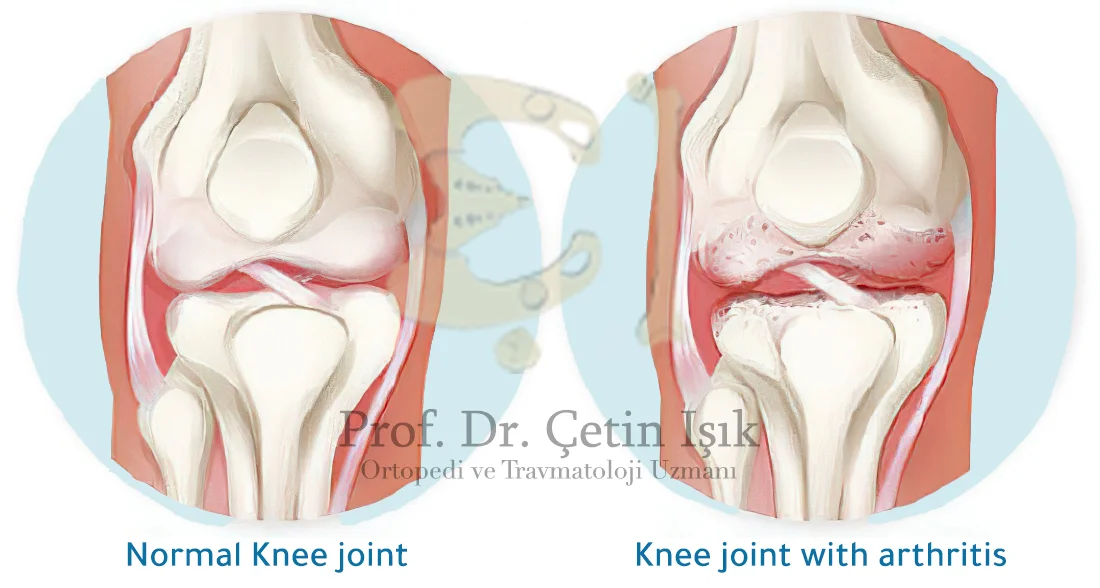
Knee arthritis can form between the femur and the tibia bone in the medial (inner) part, in the lateral (outer) part of the knee joint or under the kneecap and when all three areas are affected; It is then referred to as trigeminal arthritis.
Over time, damage to the meniscus may lead to the development or worsening of knee deformities, including bowed knee.
Knee arthritis is a very common disease that can affect all ages, with the prevalence of infection in the elderly, especially women more than men.
Types of knee arthritis
There are about 100 types of arthritis. The main common types of knee arthritis include:
Osteoarthritis: It is the most common form of knee arthritis, as it is considered one of the degenerative joint infections and often affects people aged 50 years and over. Osteoarthritis results in gradual cartilage erosion, so the protective space between the bones decreases, and bone friction occurs and may lead to the formation of bone spurs.
Rheumatoid arthritis: It is a chronic autoimmune disease, in which the body's immunity damages natural tissues such as cartilage and ligaments, and it can attack several joints throughout the body, including the knee joint, which means that it often affects both knees together.
Post-traumatic arthritis: resulting from a cartilage tear, ligament injury, or knee fracture, in which symptoms of knee arthritis may appear years after the injury.
Other forms of arthritis that affect the knees include:
- Gouty arthritis
- Reactive arthritis
- Infectious arthritis
- Arthritis in children
Symptoms of knee arthritis
In general, knee pain and swelling are among the most prominent symptoms of knee arthritis. The pain usually develops slowly and gradually despite the possibility of its sudden appearance. At first, the patient notices the pain in the morning period, when sitting, and at rest.
Other symptoms of knee arthritis include:
- A creaking or popping sound
- Difficulty walking
- Joint stiffness
- knee sprain
- Skin redness
- Feeling of heat when touching the joint
- Holding or locking the knee while moving
Symptoms of the knee joint may develop rapidly or over several years, depending on the affected person's condition. The injury may subside and stabilize for a long time and then return again.
Factors that aggravate symptoms of knee osteoarthritis include:
- Cold weather
- Pressure nervous
- Hyperactivity
Risk factors for knee arthritis
There are several causes and factors that contribute to the development of inflammation that occurs in the knee joint, namely:
- Age: As in the case of osteoarthritis, the greater the age of the person, the greater the incidence of arthritis
- Heredity: Genetic defects in the knee play a role in the occurrence of arthritis
- Weight gain: Obesity and excess weight affect the knees negatively due to bearing additional pressure Trauma: Repeated or severe injuries can lead to osteoarthritis years later.
- Gender: Postmenopausal women are more likely to develop knee osteoarthritis than men
- Autoimmune triggers: may result in activation of rheumatoid arthritis
- Developmental abnormalities: Deformities such as bowed knees and bowed legs cause additional pressure on certain parts of the knee, and as a result, knee cartilage deteriorates.
- Other health conditions: The presence of diseases such as diabetes mellitus, high cholesterol, hemochromatosis, and vitamin D deficiency increases the chances of disease occurrence.
Diagnosis of knee osteoarthritis
The doctor first takes the patient’s health history and conducts a physical examination by examining and touching the knee and asking the patient to walk on it if possible to assess the level of knee pain and the extent of its movement or the presence of any swelling and signs of inflammation in the joints.
The doctor orders some blood tests based on the patient's physical examination, such as:
- Rheumatoid factor test: This helps confirm the presence of rheumatoid arthritis
- Uric acid test: to detect gouty arthritis
To confirm the diagnosis and determine the level of recurrence, an x-ray of the joint may also be performed:
- X-rays: X-rays are used to check for signs of cartilage breakdown in the knee, narrowing of the joint space, or the formation of bony bumps. It also helps rule out other causes of pain.
- MRI: provides graphic images of soft tissues and cartilage to detect early abnormalities typical of arthritis
Other helpful diagnostic procedures that doctors may need include:
Arthrocentesis: an outpatient procedure, a sterile needle is used to take samples of joint fluid which can then be examined for infection or gout
Arthroscopy: It is a surgical technique in which a tiny camera is inserted into the patient's joint to obtain visual information about damage to the knee joint
Knee arthritis treatment
There is no definitive cure for knee arthritis, but several measures may help relieve pain and manage troubling symptoms.
Nonsurgical measures for the treatment of knee osteoarthritis
Initial treatment aims to reduce the intensity of pain and try to prevent the development of inflammation, with a set of self-care measures that include the following:
- Maintain a healthy weight to take the load off the knees
- Modify sports activities from high-impact, such as running, to low-intensity, such as cycling, with the need to do about 150 minutes of exercise during the week.
- Wear comfortable shoes and use shock-absorbing inserts
- use knee braces appropriate, which is usually remarkably effective in the presence of a knee deformity
- If the pain is severe or bothersome, crutches can be used while getting around
- It is very beneficial to adhere to a supervisor in physical therapy who helps in identifying stretching and resistance exercises to strengthen the muscles of the body, especially the leg and thigh
Alternative therapies
Certain alternative or complementary therapies may help control the pain, such as:
- Acupuncture: A specialist inserts fine needles into specific points on the body to relieve pain
- Balneotherapy: It involves placing the knee joint in warm mineral spring water
- Transcutaneous electrical stimulation: Some people use an electrical nerve stimulator to relieve pain. The machine applies a weak electric current to points on the surface of the body.
- Platelet Rich Plasma (PRP): Platelets contain growth factors that are believed to be beneficial in reducing symptoms of inflammation.
- Treatment of arthritis with stem cells: these are precursor cells that can be taken from the patient’s body and injected into his knee. They have the ability to grow into new tissues and thus heal damaged joint surfaces.
Medical therapy
The medications used to treat knee arthritis vary according to the type of inflammation and the stage of the disease, as they include:
- Acetaminophen, which is a simple over-the-counter pain reliever
- Non-steroidal anti-inflammatory drugs such as ibuprofen
- Nutritional supplements such as glucosamine chondroitin that contribute to strengthening the body's joints and bones
- Corticosteroids (cortisone injections) are not recommended by doctors in the long term due to its side effects
- COX-2 inhibitors; It is a special group of NSAIDs with fewer side effects
- Genetically modified antirheumatic drugs (DMARDs).
Surgical treatment of knee arthritis
Most often, knee surgery is the last resort for arthritis after previous measures fail to relieve pain or in severe cases that impede the patient's life.
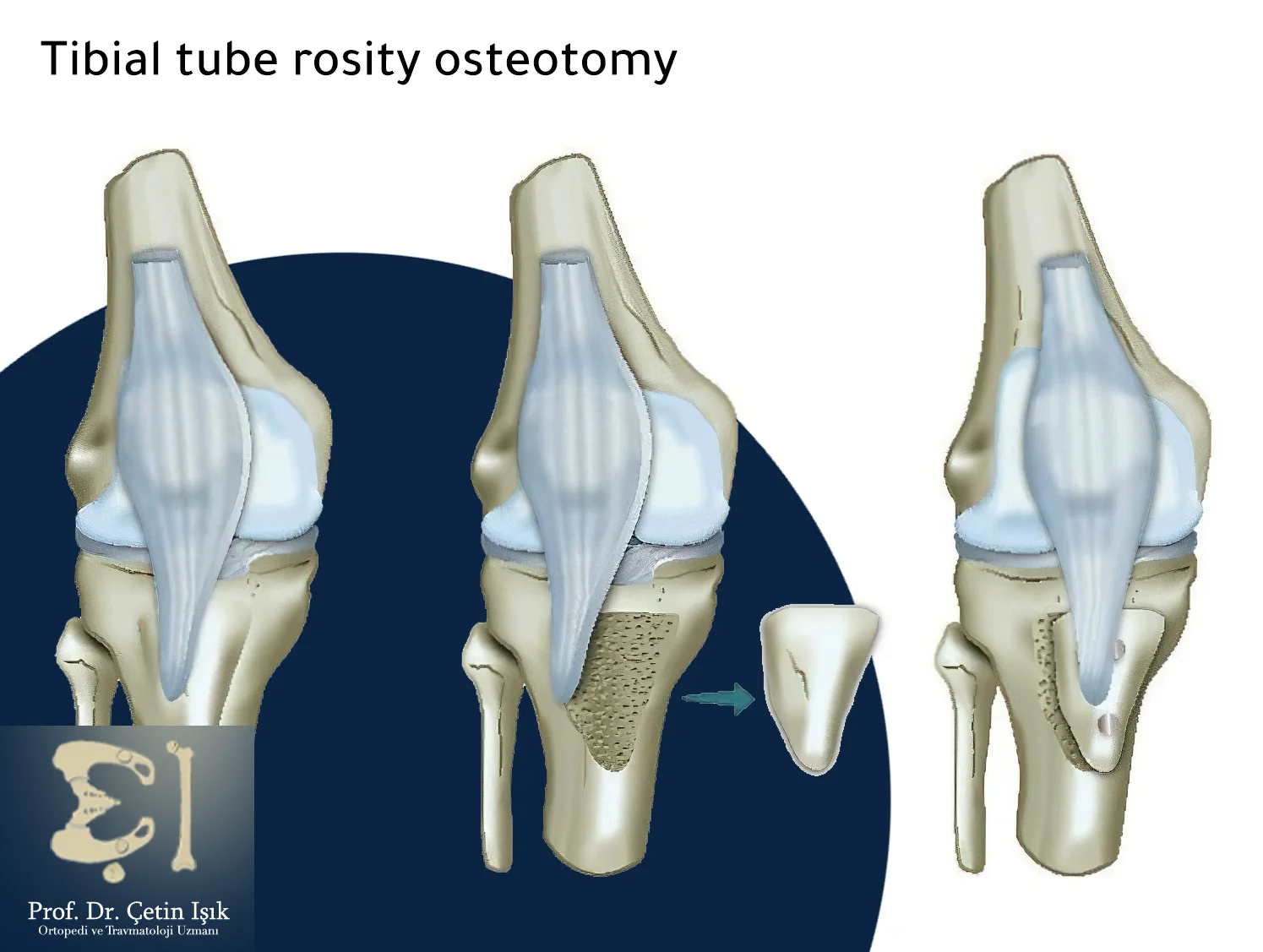
Surgical procedures include a group of options depending on the case, namely:
Arthroscopy: The surgeon inserts small tools with an endoscope into the joint to detect areas of damage, through which he can remove any bone fragments or repair ligament tears around the knee.
Cartilage grafting: The surgeon uses a cartilage graft from another joint to repair the cartilage around the knee.
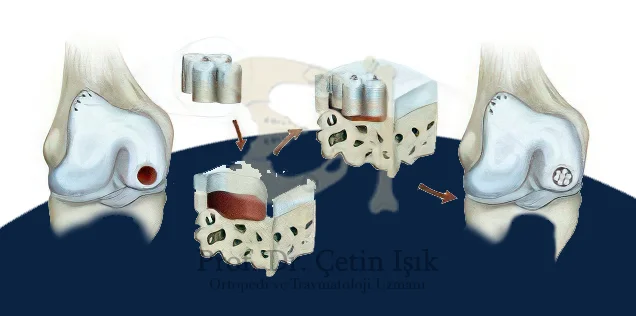
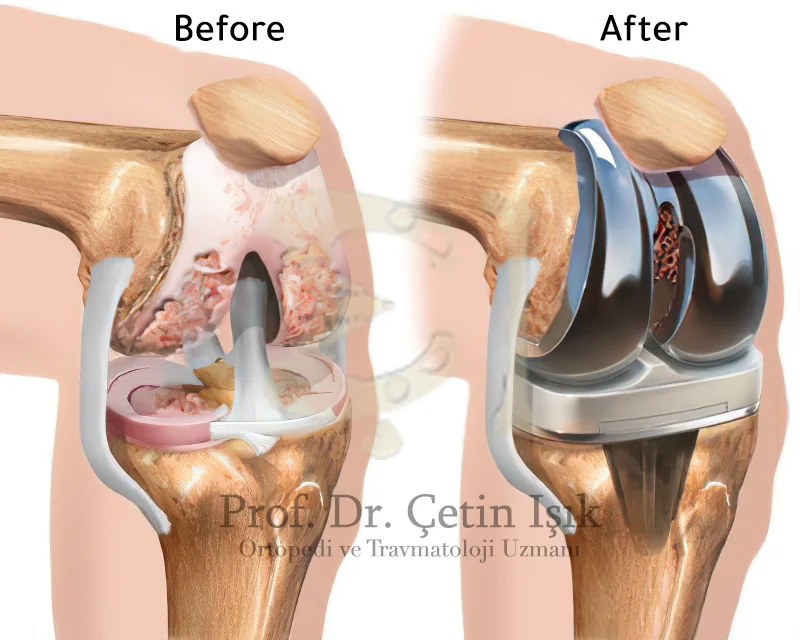
Knee joint replacement In whole or in part: the damaged joint is replaced with a metal or plastic one in case conservative treatments fail and inflammation develops until the knee joint is damaged.
There are millions of people in the world who suffer from knee arthritis, which is one of the diseases that need care and follow-up, as the knee joint is characterized by being one of the most vital joints in the body, and its inflammation causes problems that negatively affect the life of the patient; however, self-care measures and appropriate treatments can be taken Control of symptoms of inflammation.
Sources:
Common questions
Conservative treatments can control pain and inflammation, but in severe cases, surgery can permanently treat knee arthritis, taking into account post-operative care tips.
Treatments for knee arthritis vary between taking analgesic medications, treating the causative condition, following daily instructions that help relieve pain, practicing exercises that strengthen the joint, and even surgical management in the last stage.
Vitamin D is particularly important for healthy bones and joints, as its deficiency can cause osteoporosis, which may contribute to the development of knee osteoarthritis.
Walking is recommended for people with arthritis, as it helps enhance joint flexibility and reduces the risk of osteoporosis.