Psoriatic arthritis is one of the unwanted problems some psoriasis patients face, and it is the most common seronegative arthritis.
In this article, we will include all the information related to psoriatic arthritis so that you will have a first step in knowing the basics of dealing with the disease and protecting people with psoriasis from it.
Overview of psoriatic arthritis
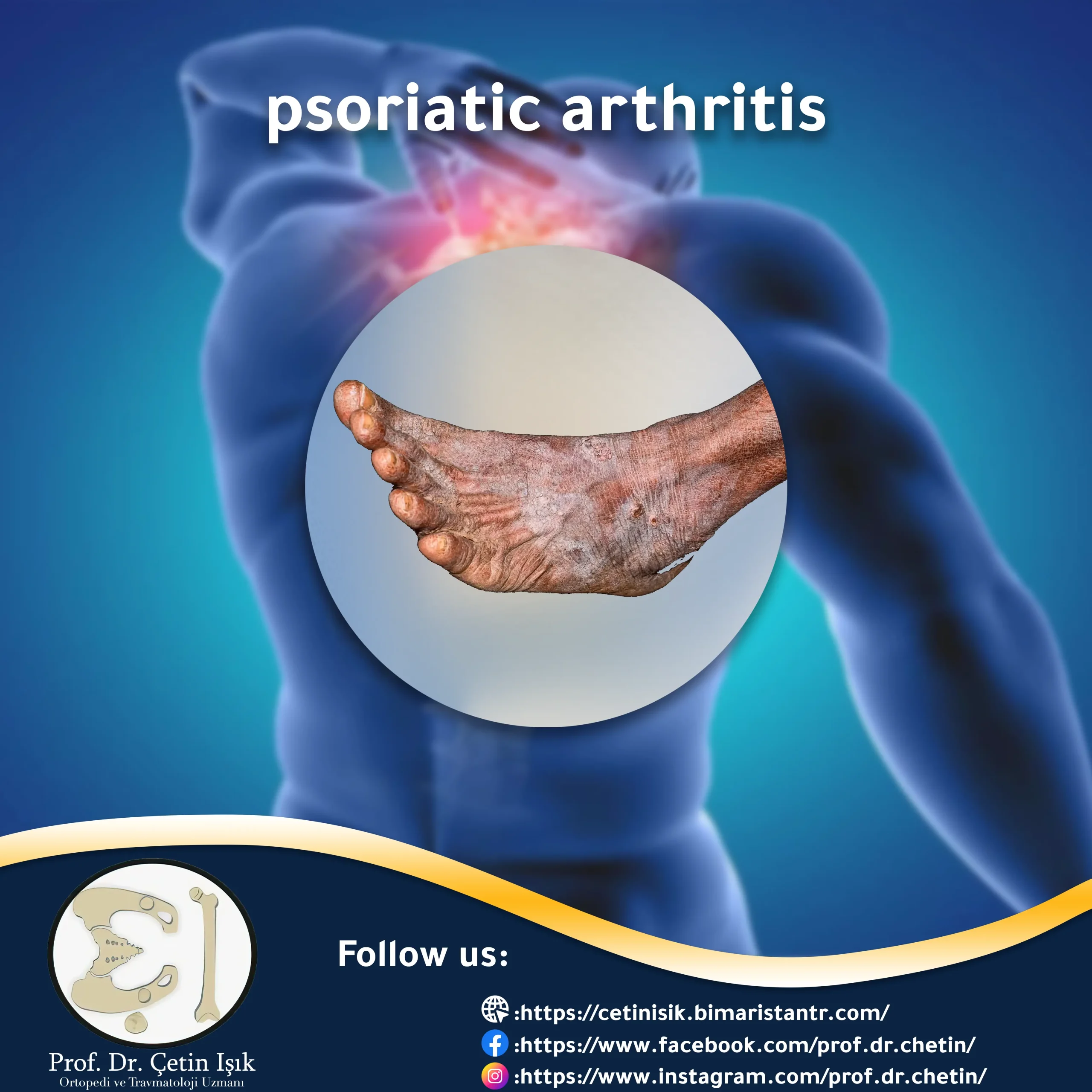
Psoriasis is a chronic skin disease caused by a problem with the immune system, in which the human immune system attacks healthy skin cells, manifesting as a rash on the skin and white scales on the skin surfaces of the hands and feet. It also affects the nails. Common psoriasis is one of the non-cutaneous manifestations of the disease; people with psoriasis suffer from it.
One out of every five patients with psoriasis suffers from inflammation in the joints of his body, and the patterns of joint injuries related to psoriasis differ from each other; the most common age at which it occurs ranges from 25 to 45 years, psoriatic arthritis often comes after the diagnosis of psoriasis, but it may come in a form Early and before the patient knows that he has psoriasis.
Psoriatic arthritis is a type of seronegative arthritis. Psoriasis of the joints results from psoriasis. The symptoms of psoriatic arthritis are similar to those of rheumatoid arthritis but differ from those in that they do not contain antibodies of rheumatoid factor found in serum, hence called serum-negative arthritis.
forms of psoriatic arthritis
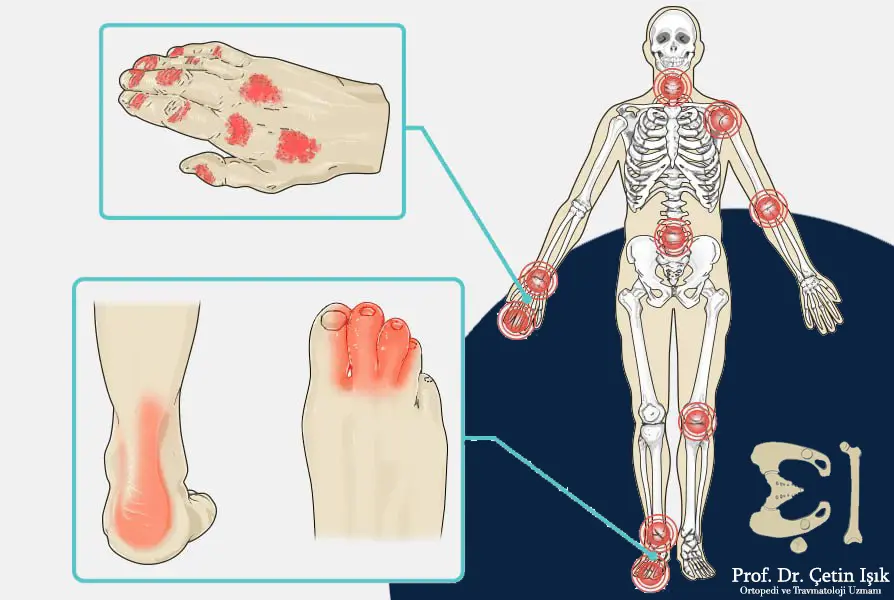
There are five main types of psoriatic arthritis:
Oligoarthritis and asymptomatic
It is the most common type, affecting the upper and lower extremities, and is characterized by the appearance of inflammation of the fingers or the so-called view of the fingers; people suffer from inflammation mainly in the joints of the knees.

Symmetric arthritis
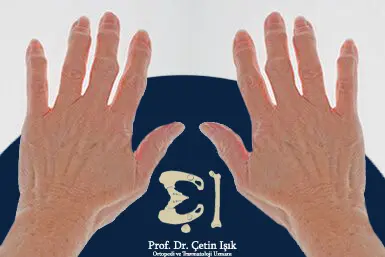
Rheumatoid disease may severely mimic and appear in the form of symmetrical arthritis affecting the small and large joints of the upper and lower extremities, but patients do not suffer from the appearance of nodules or extra-articular manifestations that characterize rheumatoid disease.
Distal interphalangeal predominant
Psoriatic arthritis is usually associated with nail dystrophy and is predominantly male.

Spondylitis in psoriasis
The clinical picture is similar to that seen in Ankylosing spondylitis But it is less severe.
Arthritis mutilans
The inflammation disfigures the joints and appears in the fingers and toes with resorption of the cartilage and bone, which leads to joint loss and instability.

Causes of psoriatic arthritis
The mechanism of arthritis in psoriasis is not yet known, but it is believed that the immune system plays a role in the development of psoriasis, and it also causes the joint inflammation that occurs with psoriasis.
Symptoms of psoriatic arthritis
Symptoms of psoriatic arthritis are characterized by an episode of intensification of symptoms followed by an episode of remission. Symptoms of psoriatic arthritis include the appearance of the following clinical signs and manifestations:
- Many injured suffer from joint pain, swelling, and inflammation, which often appears in the fingers and toes.
- Deformation of the joints due to chronic inflammation.
- Appearance of skin lesions.
- Nail changes: pitting of nails, onycholysis, and subungual hyperkeratosis.
- Uveitis: which causes eye pain with redness in addition to blurred vision, and if not treated, it can lead to vision loss.
Differential diagnoses of psoriatic arthritis
The symptoms and manifestations of psoriasis of the joints are similar to their counterparts of diseases that cause inflammation in the joints of the body, so that confusion can occur in the diagnosis if only reliance is made on the symptoms and clinical manifestations. We mention some of the differential diagnoses:
- Gout and pseudogout
- Osteoarthritis (degenerative arthritis)
- Septic arthritis (including viral and bacterial arthritis)
- Rheumatoid Arthritis
Diagnosis of psoriatic arthritis
A ratio of 60% to 80% of patients showed arthritis after psoriasis and the onset of other symptoms. However, in some less common cases, arthritis preceded the appearance of signs of dermatitis and other symptoms diagnosed with psoriasis. There is no specific test for this disease, but there are several investigations and trials that can be adopted to rule out other causes and conditions in which arthritis occurs, including:
Clinical examination
It is easy for doctors to diagnose psoriatic arthritis if the patient’s medical history is known and the patient has psoriasis by taking the patient’s clinical history or seeing skin changes in people with psoriasis. Diagnosis probability
Laboratory tests
These examinations and tests help rule out other causes of arthritis similar to psoriatic arthritis. Tests include:
- RF antibodies: are used to rule out rheumatoid arthritis or rheumatoid disease, but they are negative in psoriatic arthritis.
- ESR test: increased erythrocyte sedimentation rate means that the erythrocytes became heavier and sedimented more quickly to the bottom of the test tube; increased sedimentation rate indicates the presence of inflammation in the body, in some cases, it can be normal in some patients, the amount of elevation reflects the severity of the inflammation.
- Amniocentesis of the inflamed joint: a positive presence of uric acid is a diagnosis of gout.
radiography
X-RAY, CT, and MRI are all helpful in seeing joint damage in people with psoriasis, as these techniques show erosions with a narrowing of the joint space. Imaging may be normal.
A radiographic investigation may be requested to rule out other causes of arthritis if another joint disease is suspected.
Complications of psoriatic arthritis
In the event of a severe injury, joint damage may occur, leading to stiffness in the joints, in addition to muscle weakness due to not using them. Some recent studies indicated that this type of injury increases the risk of one of the following factors:
- Arterial hypertension
- Obesity
- Diabetes mellitus (type 2)
- Heart problems
- High blood cholesterol
- Psoriatic arthritis and pregnancy in an affected woman may result in the fetus being born before 37 weeks.
Treatment of psoriatic arthritis
Treatment for people with psoriatic arthritis aims to reduce the inflammation that occurs, and the type of treatment depends on the severity of the inflammation and the general health condition and age of the patient. Early treatment can prevent severe joint damage. Treatment plans for psoriatic arthritis include:
Simple home remedies
- Rest
- Apply cold compresses
Psoriatic arthritis medications
- Methotrexate: This is the treatment of choice for severe psoriasis.
- Simple analgesics and NSAIDs help relieve pain and improve symptoms.
- Intra-articular corticosteroid injections help control severe inflammation of the synovial membrane.
- Biological therapies are used to reduce inflammation.
Surgical treatment
It involves repairing or replacing the damaged joint, but doctors rarely resort to it until years after diagnosis or severe joint damage.
Physical rehabilitation
It includes therapeutic exercises to strengthen muscles or restore muscle movement as before.
Herbal arthritis treatment
Herbs like ginger and turmeric contain anti-inflammatory properties.
Prevention of psoriatic arthritis
Many medications worsen psoriasis attacks, including:
- lithium
- Sudden discontinuation of corticosteroids
- Beta-blocker medications
- Malaria medicines
Therefore, you must stop using these types of medicines and tell the treating doctors if you are taking them
Other preventive measures include:
- Rest
- Playing sports
- Splints and other supports
In conclusion, 20% of patients with psoriasis get psoriatic arthritis, including five primary forms. In a few cases, arthritis precedes other symptoms of psoriasis. Diagnosis can be made by excluding other similar diseases. Treatment is conservative, and surgery is rarely resorted to.
Sources
Common questions
A quarter to a third of psoriasis patients develops inflammation or arthropathies, which are called psoriatic arthritis, a condition that causes pain in the joints.
Psoriatic arthritis is not considered a fatal disease because it affects the skin, nails, and joints and causes disease symptoms in them, but it does not affect the body's vital organs. The side effects of psoriatic joint disease medications can pose some risks, but they can be avoided if you follow up on treatment with the doctor and adhere to his instructions.
Psoriatic arthritis is a chronic disease in which no specific medicine causes complete recovery. Still, it is possible to live with this condition and adhere to the treatment recommended by doctors to reduce the severity of symptoms and follow a sports regime and practice exercises that help avoid Severe joint injuries.
Psoriasis can cause an increased risk of a form of skin cancer, particularly the squamous cell type as well as the basal cell type.